New Stem Cell Treatment May Cure Type 1 Diabetes
In a paper published in the journal Cell, Douglas Melton announces that he has created a virtually unlimited supply of the cells that are missing in people with type 1 diabetes.
By replacing these cells—and then protecting them from attack by the body’s immune system—Melton, now a professor and stem cell researcher at Harvard, says someday he’ll have a cure.
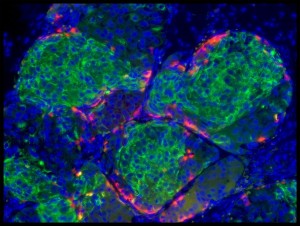
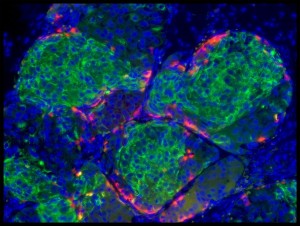
In type 1 diabetes, which usually starts in childhood, the person’s immune system attacks and destroys beta cells in the pancreas. Melton used stem cells to manufacture a new supply of these beta cells, which provide exquisitely fine-tuned responses to sugar levels in the blood.
Since the 1920s, people with type 1 diabetes have been kept alive with insulin injections, though many still face nerve damage, slow wound healing, and even blindness because even the best pumps and monitors are not as effective as the body’s beta cells.
The only known cure for type 1 diabetes is a beta cell transplant, which takes the cells from someone who has recently died. But the procedure is complicated, and the patient must remain on drugs forever to prevent the immune system from destroying the cells.
Fewer than 1,000 beta cell transplants have ever been done, said Albert Hwa, senior scientific program manager for beta cell therapies at the diabetes research organization JDRF.
Melton, with the help of about 50 graduate students over the past 15 years, has now managed to create replacement beta cells that—at least in rodents—seem to be nearly as good as the real thing. Human testing will probably begin in two to three years, he said.
It’s not yet clear whether one dose of 150 million or so beta cells would be enough to last a lifetime, or if additional doses would be needed.
The researchers started with cells taken from a days-old human embryo. At that point, the cells are capable of turning into any cell in the body. Others have tried to make beta cells from these human embryonic stem cells, but never fully succeeded. Melton’s team spent a decade testing hundreds of combinations before finally coaxing the stem cells into becoming beta cells.
The technique also works using stem cells that don’t require destroying an embryo, avoiding what has been a highly controversial step. The other cells are called induced pluripotent stem cells; they are adult cells that are turned back into stem cells. Then the stem cells can be developed into beta cells.
Both types of artificial beta cells could also be used to treat the roughly 10 to 15 percent of people with type 2 diabetes who are dependent on insulin shots, or to help those with type 2 avoid the need for insulin, Melton said. Because type 2 diabetes is not an autoimmune disorder—it’s usually connected to obesity—the body will not destroy replacement cells.
Combined, more than 300 million people worldwide have type 1 or type 2 diabetes, according to the World Health Organization.
Breaking Through Barriers
The work also helps confirm the promise of stem cell research, which was heralded in its early days as a source of cures for diabetes, paralysis, heart disease, and Alzheimer’s.
Making new cells provides “half the solution to the problem” of type 1 diabetes, Melton said. The other half is protecting those cells from rejection by the immune system once they’re implanted. Melton is working with MIT applied biology professor Daniel Anderson to design an implantable device that would work like an inkjet printer, coating the cells in an algae-like substance so immune cells can’t stick to them.
Melton said it will take at least another year of work to be able to produce cells the government would consider for testing in people. He predicts it will take an additional two years of testing before his approach could begin helping large numbers of patients.